Biomechanics of Fracture Healing
Researchers: D Epari, M Schuetz
An improved understanding of bone regeneration mechanisms represents a significant opportunity to improve quality of life and reduce the economic burden associated with extended disability arising from fracture non-unions.
The impairment of the healing process has been dependent on both the biological and mechanical environment. Understanding the mechanobiology of bone healing has been hampered by limitations in the ability to control the mechanical boundary conditions during bone healing.
This study utilises a highly innovative experimental bone healing model and active fixation system that enables precise control of the mechanical environment and real time monitoring of the progression of healing. The application of this model will allow the investigators, for the first time, to investigate clinically relevant research questions such as the effect of single extreme loading events on healing, and the potential for intelligent and adaptive fixation devices to accelerate healing.
In combination with computational modelling approaches, this study will lead to an enhanced understanding of the influence of the mechanical environment on bone healing. The research has the potential to inform the development of new fixation strategies, rehabilitation protocols and to lead to novel therapeutic treatments for bone regeneration.
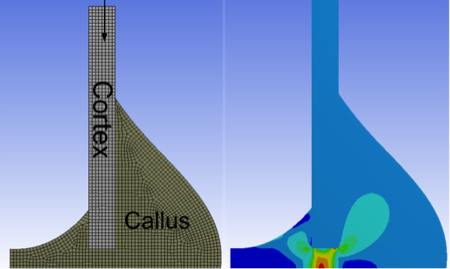
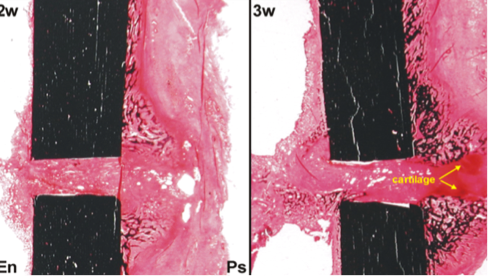
Figure 1: Coupling computer models with tightly controlled boundary conditions, in experimental models of bone healing, allows the influence of the mechanical environment to be elucidated on the biological processes of bone healing.
Wrist Fractures in the Elderly
Researchers: IA Harris, JM Naylor, Z Balogh, P Smith, H Drobetz, M Richardson, M Chehade, C Morrey, N Ward, C Hoffman, G Smith, R Walker, J Mulford, A Oppy, M Wren, W Xuan, K Howard, P Tamblyn, M Gupta, B Schick, I Incoll, I Elkinson, S Viswanathan, H Lombard, P Tran, A Hatfield, R Buchbinder, R Ivers
Displaced fractures around the wrist in older patients represent one of the most common fractures treated by orthopaedic surgeons, yet treatment methods vary widely: the two most common methods being fixation with a plate (requiring admission to hospital and surgery), and manipulation of the fracture and immobilisation in a plaster cast (which may be done as an outpatient, in the emergency department).
There is currently very little high quality scientific evidence to guide surgeons on the best treatment, given the variety of costs, risks and benefits between these two very different treatment alternatives.
A large group of researchers from across Australia and New Zealand have come together to answer this question with a multicentre randomised trial comparing these two treatments. This study will address a large gap in the evidence around the treatment of this common fracture.
Outcomes of Arthritis Surgery
Researchers: P Choong, M Dowsey
Musculoskeletal disorders are the second largest global contributor to years lost through disability. Osteoarthritis of the hip and knee is the third most prevalent condition in this group of disorders.
Under the leadership of Prof Peter Choong and Dr Michelle Dowsey, a high fidelity surgical database at St Vincent’s Melbourne Arthroplasty and Outcomes (SMART) registry has been maintained, since 1998. The registry provides material for analysing the various patient, prosthetic and treatment factors that impact patient outcomes and prosthesis survival.
The SMART registry has been central to identifying risk factors for poor surgical outcomes and providing the foundation for our program of research. We lead a program of research that aims to improve access to and outcomes from total joint replacement in collaboration with a team of national and international experts in:
- arthritis surgery
- outcomes research
- primary care
- mental health
- infectious diseases
- biomechanics
- rehabilitation
- health economics and risk analysis
- implementation science
- health workforce
- health service delivery